Contents
- 1 Rheumatoid Arthritis Pathophysiology
Today we looked at Rheumatoid Arthritis Pathophysiology, the clinical manifestations, the hand involvement, the potential causes as well as articular manifestations of rheumatoid arthritis.
Rheumatoid Arthritis Pathophysiology
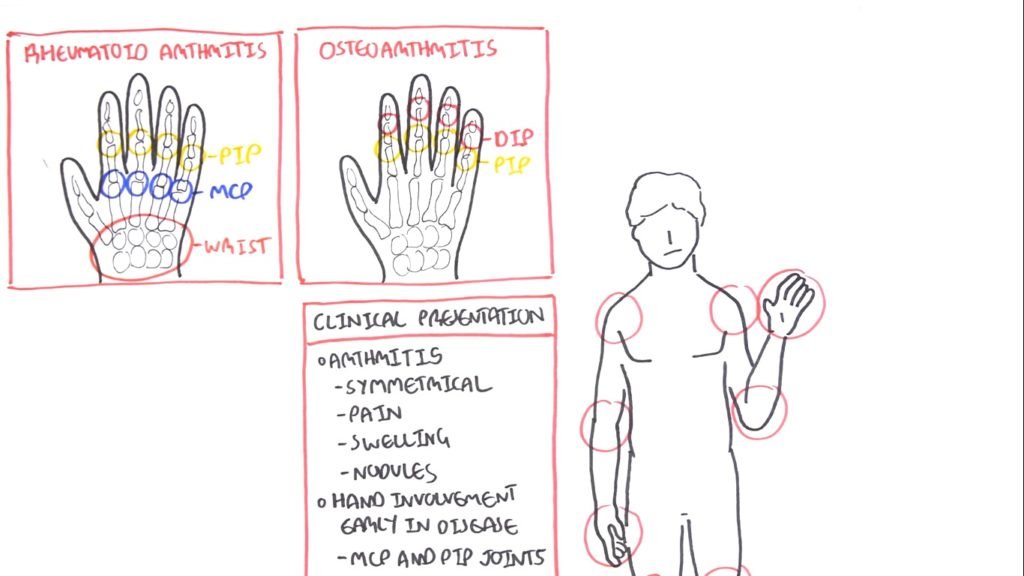
The clinical presentation of rheumatoid arthritis is symmetrical. The patient has pain, swelling as well as nodules around the area. Hand involvement is early in the disease and affects the metacarpophalangeal and proximal interphalangeal joints.
Hand Involvements
First, let us look at the hand involvement in rheumatoid arthritis. See how it differs in Rheumatoid Arthritis vs Osteoarthritis. So in osteoarthritis, the joints affected are the distal interphalangeal joints as well as proximal interphalangeal joints. In rheumatoid arthritis, it is proximal interphalangeal joints and the metacarpophalangeal joints.
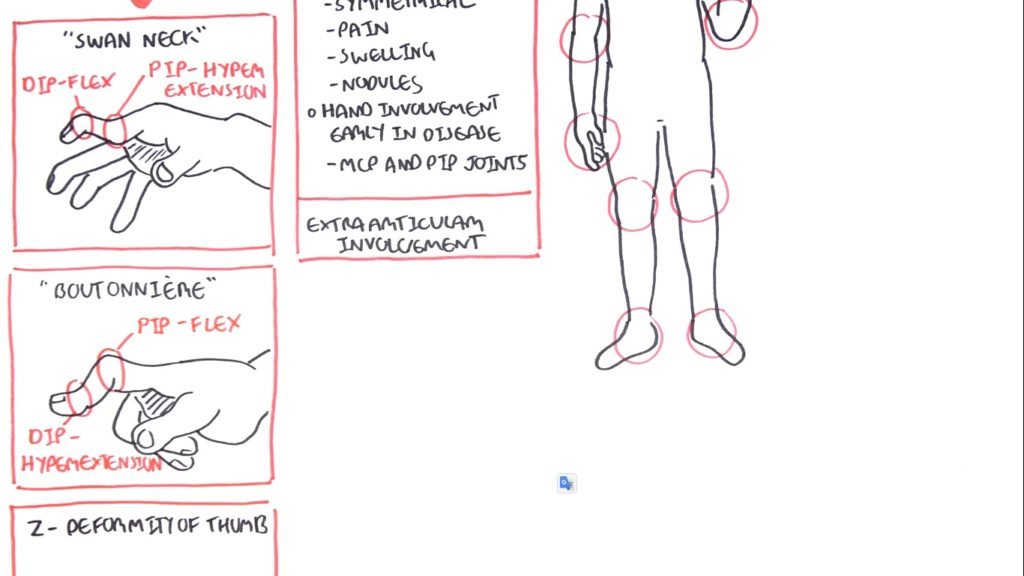
As the disease progresses, other symptoms start occurring in the hands. These are swan-neck, boutonniere or z-deformity of the thumb.
- Swan-Neck
So in swan neck what you have is you have the distal interphalangeal joints flexed but the proximal interphalangeal joints hyperextended. In boutonniere, it’s the opposite. You have the distal interphalangeal joints hyperextended and the proximal interphalangeal joints flexed.
- Z-deformity
The z-deformity of the thumb is essentially the thumb looking like a Z. In the hands, the hands can also deviate medially. This is called ulnar deviation.
Anatomy of Rheumatoid Arthritis
We have the bone, the joint capsule, the synovial membrane also known as synovium. The synovial membrane is also known as synovium, which produces the synovial fluid which helps in lubrication as well as supplying nutrients to the area. In rheumatoid arthritis pathophysiology, you essentially have inflammation of the synovium of the synovial membrane. You have a sign of synovitis. This causes pain and swelling which occurs in rheumatoid arthritis.
- Bone and Cartilage Erosion
This also leads to bone and cartilage erosion breakdown. Another feature we can see in the joints of rheumatoid arthritis patients is angiogenesis.
The synovial membrane is made up of these cells known as fibroblast-like synoviocytes (FLS). These are very important in the pathogenesis of rheumatoid arthritis.
- TNF Alpha, Interleukin 1 & 6
Now the exact trigger of the information of the disease is really not quite known. However, we are now looking at what cells we can find here and what cells are involved. So we have macrophages here. They essentially begin creating cytokines such as TNF alpha, interleukin 1, and interleukin 6, which of course leads to inflammation.
Cytokines
These cytokines also stimulate fibroblasts like synoviocytes. When the fibroblasts like synoviocytes are stimulated, they essentially become activated. They begin to proliferate. At the same time, they also begin assisting in that rank El expression stimulating the RANKL expression which together with the cytokines here will stimulate osteoclast activity which will lead to bone erosion what we find in rheumatoid arthritis pathophysiology.
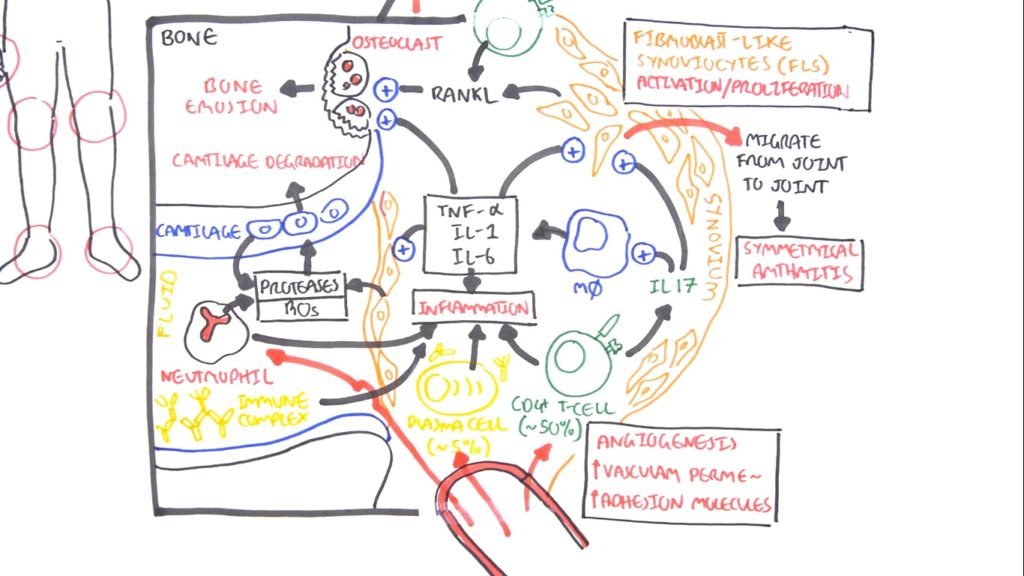
When the fibroblasts like synoviocytes are stimulated and proliferate, they also begin secreting proteases. These proteases essentially cause the cartilage to break down. So we get cartilage degradation. The cartilage also secretes proteases and it’s sort of like a feedback loop.
Joint to Joint
Another interesting feature of when of the fibroblasts like cartilage is that when it’s stimulated what it’s activated, these guys can actually migrate from joint to joint. So they can migrate from the hand joint on one side to the hand joint on the other. This is why we get symmetrical arthritis in rheumatoid arthritis.
T-Cells in Rheumatoid Arthritis Pathophysiology
We also can find t-cells in the area in the synovium. T-cells make up about 50% of the immune cells in this area. So they are very important in pathophysiology. T-cells are promoted inflammation essentially, and they secrete they can secrete interleukin 17 which will promote macrophage activity as well as stimulate the fibroblasts like cartilage. The T-cells also help in the expression of RANKkL which stimulate osteoclast for bone erosion.
- Plasma Cells
We also find plasma cells in the area. Plasma cells only make up a small majority about five percent of the immune cells. They essentially assist in in inflammation through cytokines as well as through antibodies. Now in the fluid in the synovial fluid, we can find neutrophils. Neutrophils they essentially produce proteases and reactive oxygen species which will essentially cause bone and cartilage degradation erosion. So they contribute to inflammation.
- Synovial Fluid
In the synovial fluid, we also find the immune complexes, which is a feature of rheumatoid arthritis. These complexes are essentially antibodies that bind to one another. They essentially promote inflammation. So those are the cells that we can find in an inflamed joint in rheumatoid arthritis.
- Angiogenesis
Again another feature or are this areas that we see angiogenesis. Also, the cytokines that are produced by all these cells help increase vascular permeability and expression of adhesion molecules on the vasculature. Allowing for these immune cells to migrate into the joints.
Cells, Migration, Root Cause?
Where do all these cells come from? Why do they migrate into these joints, and cause root rheumatoid arthritis?
Well, as I mentioned we don’t actually know but there are a few theories out there. So let’s go to the pre-rheumatoid arthritis phase before a person has rheumatoid arthritis. There are many possible things that could contribute to the development of rheumatoid arthritis pathophysiology.
- Reasons for Rheumatoid Arthritis
These include genetics, epigenetic modifications, smoking, a bacteria called porphyromonas gingivalis which can lead to gingivitis. Essentially these things they can cause modification of autoantigens. what do I mean by modifications of autoantigens? It essentially means is a modification of your own antigens to make it seem foreign to the immune cells.
Citrullination
So not only these things can occur in the joints such as you can have a synovial injury or hyperplasia or you can have an infection or within the joint. This will trigger you know cytokine release and it will cause inflammation. This inflammation that occurs in the joints can also lead to modification of autoantigens. So, modification of your own antigens making it seem foreign. This also includes citrullination.
CD4 T-Cell Activation
So because you have modifications of your own antigens this will be recognized by antigen-presenting cells. It will essentially activate the antigen-presenting cells to initiate an immune response. The antigen-presenting cell will migrate to the lymph nodes where the antigen-presenting cell will activate T-cells here in the area. So we can have a CD4 T-cell activation. When the CD4 when the T cell is activated it can activate them B cells in the germinal center and this can be through co-stimulation.
B-Cells
When the B cells are activated they will begin to class switch and they will become plasma cells. Plasma cells will then produce Autoantibodies. They will produce the antibodies against your own antigen essentially.
So then what? Well, you have now CD4 T-helper cells, the antibodies, and the plasma cells. They will also have homing receptors which will allow them to migrate to join tissue. So that is how they move into the joints in rheumatoid arthritis.
IgM Antibody
Now it’s important to talk about the antibodies because they are an important feature in rheumatoid arthritis pathophysiology. We have two main antibodies found and these are we look at one of them at a time. So the first one is the rheumatoid factor, which is an IgM antibody. It’s present in 75 percent of people with rheumatoid arthritis.
Rheumatoid Arthritis Immunology
What these guys do is that they target FC portion of our IgG antibodies and so the constant region. They essentially are the ones that are that that in that form the immune complex and can deposit in the synovial fluid. The rheumatoid factor not only forms immune complexes with but with itself but with the IgG as well as complement proteins. So it will promote inflammation.
- Anti-Citrullinated
The second antibody is the anti-citrullinated of our protein antibody. Now, these guys as the name suggest they target citrullinated proteins. These are things such as fibrin and filaggrin. They target citrullinated proteins.
- What are they?
Well, citrullinated proteins are essentially proteins who have our arginine residues that have been converted to citrullinate. This sort of change deems makes it seem foreign to the body. That is why when we have modifications of our autoantigens such as citrullination our body thinks it’s foreign.
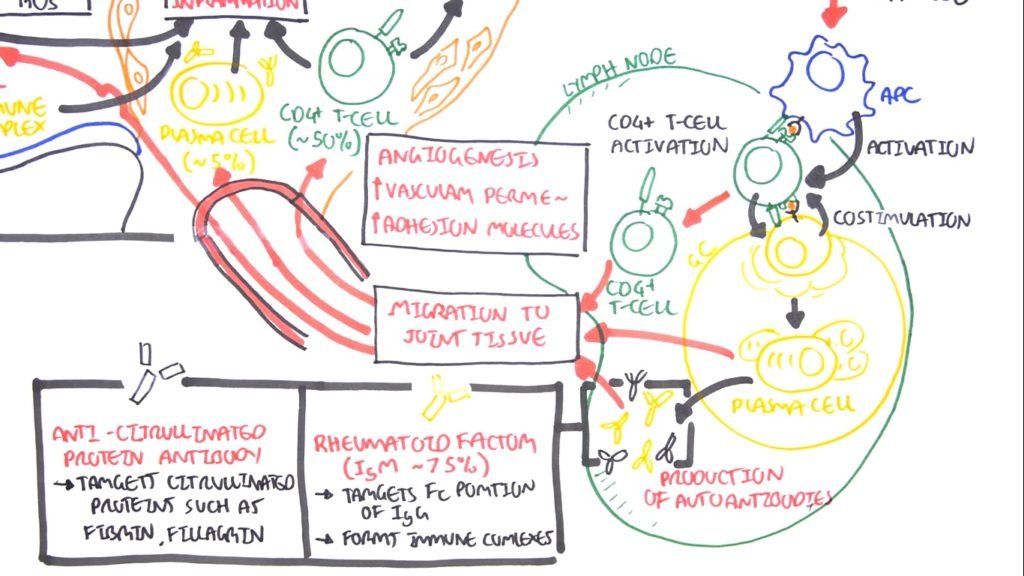
Linking to Pathophysiology
Unfortunately, in our joints, we have these sorts of tissues. Therefore, that’s how this antibody contributes to rheumatoid arthritis pathophysiology.
Essentially this rheumatoid factor and Angie citrullinated protein antibodies they’re important for in helping diagnose rheumatoid arthritis. Not everyone has a rheumatoid factor but the anti-citrullinated protein antibody it is a lot more specific for rheumatoid arthritis pathophysiology.
Extra-Articular Involvement
Now, it’s important that we talk about the extra-articular involvement within rheumatoid arthritis. So, what I’m talking about is the involvement of other organs around the body and how rheumatoid arthritis causes problems there too.
These are mainly in TNF alpha interleukin 1 and interleukin 6. So within the blood, we have increased inflammatory cytokines. They essentially contribute to many things around the body.
CRP or ECR
For example, in the skin, they contribute to the nodule formation. In the liver, it will begin producing more CRP or ECR proteins which are inflammatory markers. The liver will produce a lot more hepcidin which will contribute to anemia in rheumatoid arthritis. Cardiovascular involvement, these cytokines and this inflammation that’s occurring will actually promote, and can also lead to promote myocardial infarction as well as stroke.
Neurological Involvement
Neurological involvement includes fatigue and depression. Musculoskeletal involvement is very serious in rheumatoid arthritis. These include osteopenia, which can lead to osteoporosis. In the muscles, the influent inflammation causes can lead to insulin resistance which can result in muscle weakness. Bone marrow involvement we can have thrombocytosis which is a lot of platelets which can contribute to plaque as well as we have anemia.
- Overview
So those are the extra-articular involvement of rheumatoid arthritis pathophysiology. You also have lung involvement such as polar effusion and lung infection. This can be attributed to the rheumatoid arthritis treatment used for mature arthritis which involves glucocorticoids. As we know glucocorticoid suppresses the immune system.
Reference
This content is strictly an overview of rheumatoid arthritis pathophysiology and is for informational and educational purposes only. Neither the sources of this content nor the publisher of this content takes responsibility for possible health consequences of any person or persons reading or following the information in this educational content. All readers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any medication.
- Feedback
Let us know what do you think about it? Leave your comments below.



